Neuropathic Pain Treatment
An Unmet Medical Need
- Chronic pain is a condition caused by a primary lesion or dysfunction of the nervous system.
- Neuropathic pain global prevalence is high, affecting 8 % of the adult population.
- Increasing socio-economic burden associated with chronic pain
- Neuropathic pain is highly resistant to the classical pain killers, with only 50% of responders to the first-line treatments.
- There are concerning safety risks with available pain drugs, notably with opioids.
Central Sensitization Mechanisms of Pain
This Central sensitization modifying agent (CSMA), stands out for its safety profile, as NDMC improve neuropathic pain without sedation, It is thus less likely to make you feel sleepy or drowsy diminishing systemic toxicity.
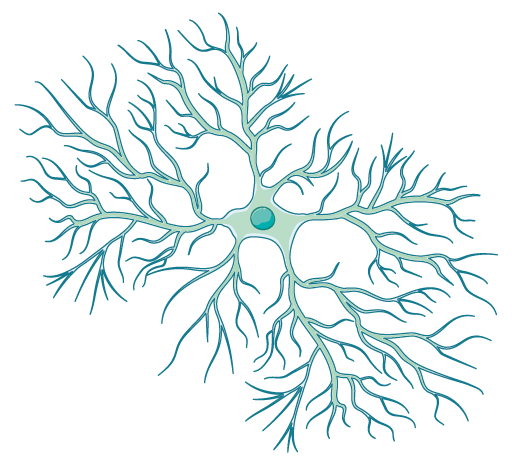
Neural excitation/inhibition imbalance
Alles SRA & Smith P. Pharmacol Rev. 2018
- GABA-receptor activation supports synaptic modulation.
Differential Allosteric Modulation of the GABAA Receptor
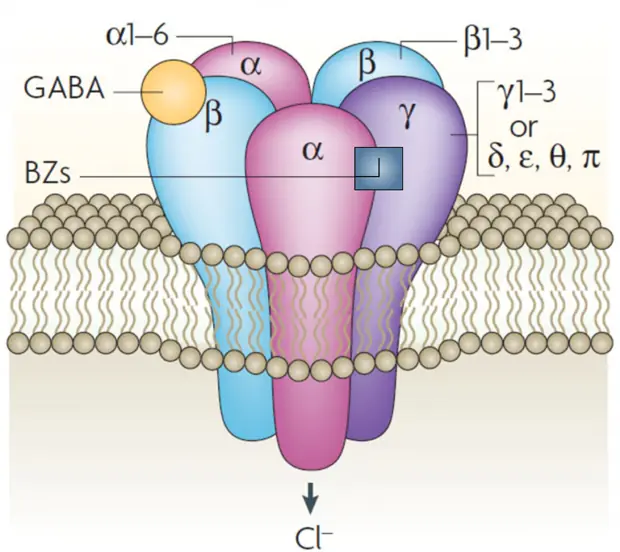
| Effect | Subunit(s) |
|---|---|
| Antihyperalgesic | α2 > α3 |
| Anxiolytic | α2, α3 |
| Myorelaxant | α2, α3, α5 |
| Anticonvulsivant | α1 |
| Sedative | α1 |
| Memory | α1, α5 |
| Dependance | α1 |
Jacob, T. C. et al. Nat Rev Neurosci. 2008
Nutt, D. J. et al. Neuropharmacology. 2007
Tan, K. R. et al. Trends Neurosci. 2011
- Modulation of GABAA receptor is key for an increased synaptic inhibition.
- Modulation of the α2 subunit is responsible for the antihyperalgesic (pain relief) effect.
- The α1 subunit activation induces sedation.
IRX-001 (NDMC)
IRX-001 (NDMC) is a first in class differential allosteric modulator of the GABAA receptor.
IRX-001 Preclinical Data
Preclinical models have demonstrated the efficacy of NDMC in treating central pain sensitization and phase 1 and early phase 2 human clinical trials suggests a concentration dependent analgesic effect on central sensitization with a promising safety profile.
Dose-dependent antihyperalgesic effect in mice neuropathic model
|
Paw withdrawal threshold (g)
|
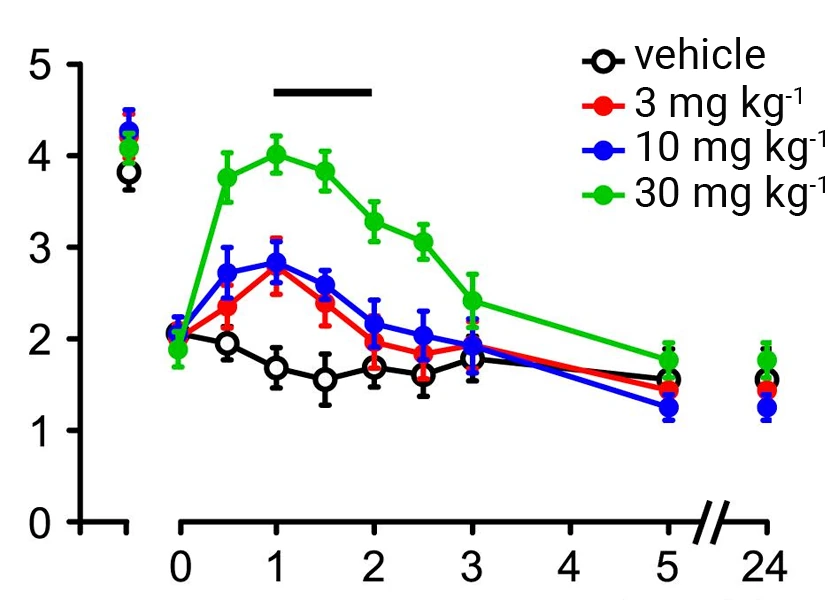
|
|
preCCI
time (h) |
|
% Maximal possible effect
|
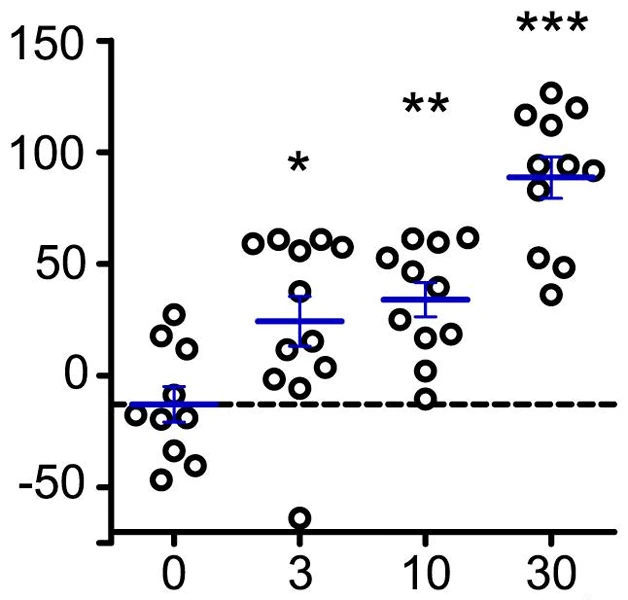
|
|
Dose NDMC (mg kg-1) |
Ralvenius et al. Neuropharmacology. 2016
Di Lio et al. Neuropharmacology. 2011
- Dose-dependent antihyperalgesia with IRX-001
- In vivo mice neuropathic pain model
Mobility/Sedation: no effect of IRX-001 whatever the dose
|
Beam crosses
|
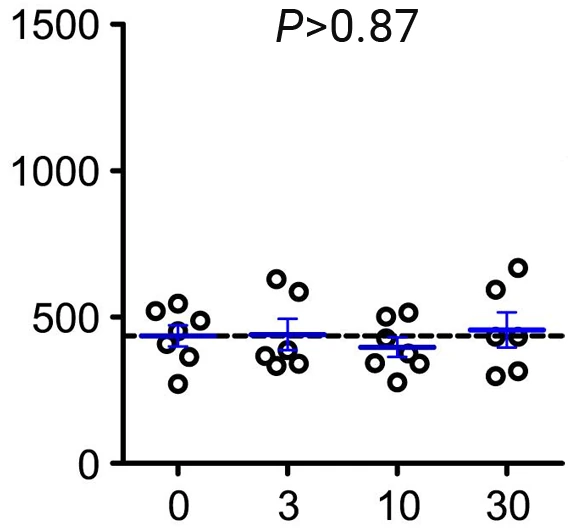
|
|
Dose NDMC (mg kg-1) |
Ralvenius et al. Neuropharmacology. 2016
Di Lio et al. Neuropharmacology. 2011
- IRX-001 does not induce sedation.
Many chronic pain states are accompanied by diminished synaptic inhibition at the spinal cord level. Conversely, pharmacological enhancement of GABAergic inhibition in the spinal cord reverses pathologically increased pain sensitivity (hyperalgesia) in experimental models of chronic neuropathic pain.
On the therapeutic side, there are only a few alternatives (pregabalin, gabapentin, duloxetine and certain opioids) which are efficacious for the treatment of chronic pain or spontaneous on-going pain. In most cases, those drugs are only partially active and have important side effects which limit their use.
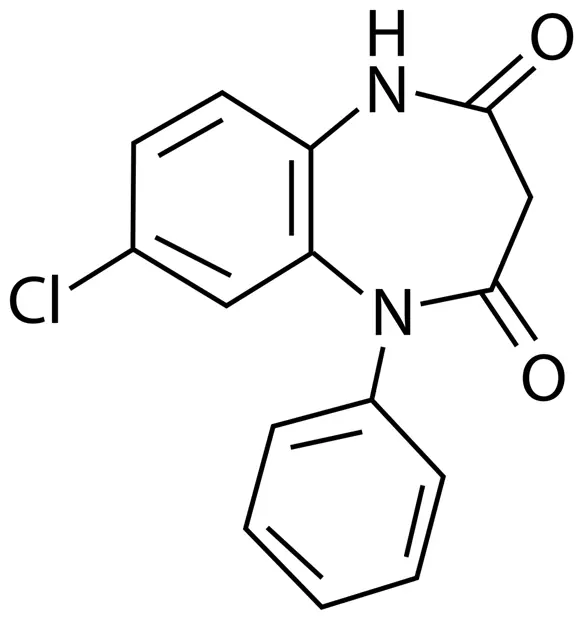
Non selective benzodiazepines carry a number of disadvantages such as ataxia, daytime (carry-over) sedation, loss of coordination, and impaired memory and cognition and an important safety consideration related to the prolonged use of non selective benzodiazepines is the development of tolerance, which increases the risk of physiological dependence.
Specific pharmacological effects of benzodiazepines are thought to be associated with their degree of affinity for different subtypes of GABAA receptors found in the central nervous system. For instance, the anxiolytic and anticonvulsant properties of benzodiazepines are mainly mediated by the activation of the α2 and α3 subunits of the GABAA receptor while tolerance and sedation which remain major impediments to their use are associated with the α1 subunit.
Functional neuroimaging and site-directed mutagenesis have provided powerful insights into the pharmacological properties of GABAA receptor subtypes.
Therefore, the main focus of the entire pharmacological benzodiazepine-oriented research was to try in the past twenty years to identify α1-sparing compounds. While the lack of activity at α1-GABAA receptors avoids unwanted sedative effects, initial compounds were not pursued while the dose needed to reach substantial efficacy led to a loss in the benefit of their selectivity.
Clobazam is a 1-5 benzodiazepine prescribed as an anti-anxiolytic agent and as adjuvant treatment for epilepsy and exerts less cognitive and psychomotor side effects compared to other benzodiazepines such as clonazepam. Clobazam is known to have higher binding affinity for α2 versus α1 receptor complexes, a difference which is shared by one of its metabolite N-desmethylclobazam, or NDMC and which is not observed with other benzodiazepines.
We showed that NDMC binds to this α2 preferred site and acts as a positive allosteric modulator, potentiating the fast inhibitory effects of GABA on neurotransmission. In addition, NDMC possesses an improved α2/α1 GABAA receptor selectivity ratio compared to clobazam.
Thus NDMC is the ideal modulator of this new target in the treatment of neuropathic pain.
NDMC exerts significant analgesia against neuropathic pain at non-sedative doses.